What is the Female Pelvis?
The female pelvis is the largest bone formation in the body. It’s a basin-shaped structure that connects to the fifth lumbar vertebra above. is also called the bony pelvis or pelvic girdle (bone belt).

Functions
- Muscle attachment – attach both the trunk (upper part of the body above the waist region) and limb muscles together
- Birth canal framework – forms the skeletal structure of the birth passage
- Organ protection – contains and protects pelvic organs
Importance to Midwifery
- Fetal passage – serves as the pathway for the baby from uterus to vulva
- Weight transmission – transfers body weight through the pelvis to the legs
- Labor assessment – pelvic measurements help determine if vaginal delivery is possible
- Positioning during birth – understanding pelvic shape guides optimal maternal positions
- Complication prevention – identifies potential obstructed labor or need for cesarean section
- Pain management – knowledge of pelvic anatomy helps explain labor pain patterns
- Postpartum care – understanding pelvic changes helps with recovery and rehabilitation
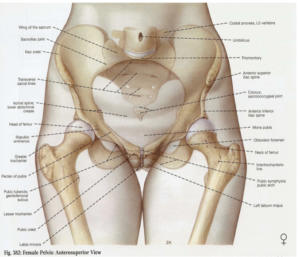
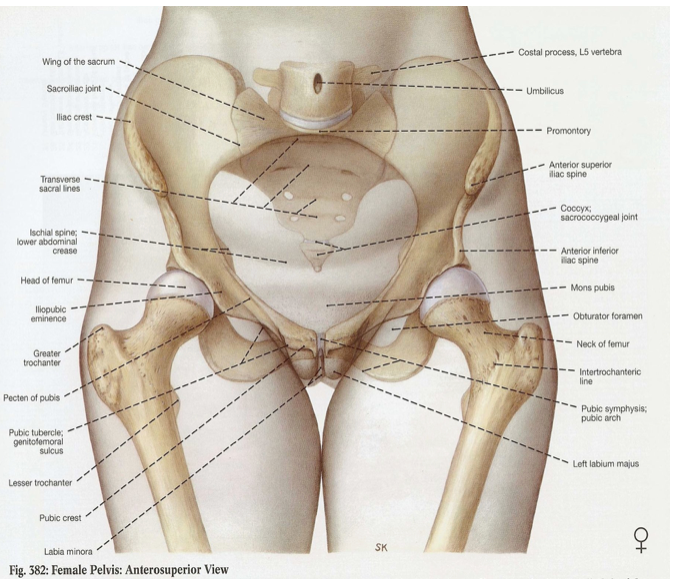
Components of the Pelvis
The pelvis has three parts:
- Two Innominate bones ( hip bones)
- Sacrum (the big triangle bone at the bottom of your spine)
- Coccyx (your tailbone – the tiny bone at the very bottom)
1. Innominate bone
Each innominate bone consists of three fused parts that meet at the acetabulum (hip socket):
- Ilium (upper part
- Ischium (lower back part )
- Pubis (lower front part)
Acetabulum a cup shaped cavity where your leg bone (femur) fits in
The obturator foramen is a triangular opening below the acetabulum where nerves pass through. It’s the space enclosed by the body of the pubic bone, the rami and the ischium.
a. Ilium
It consists of two parts;
Upper part which forms the iliac crest – the bony ridge you can feel when you put your hands on your hips and Provides attachment for abdominal muscles
The Lower part which forms the upper two-fifths portion of the acetabulum
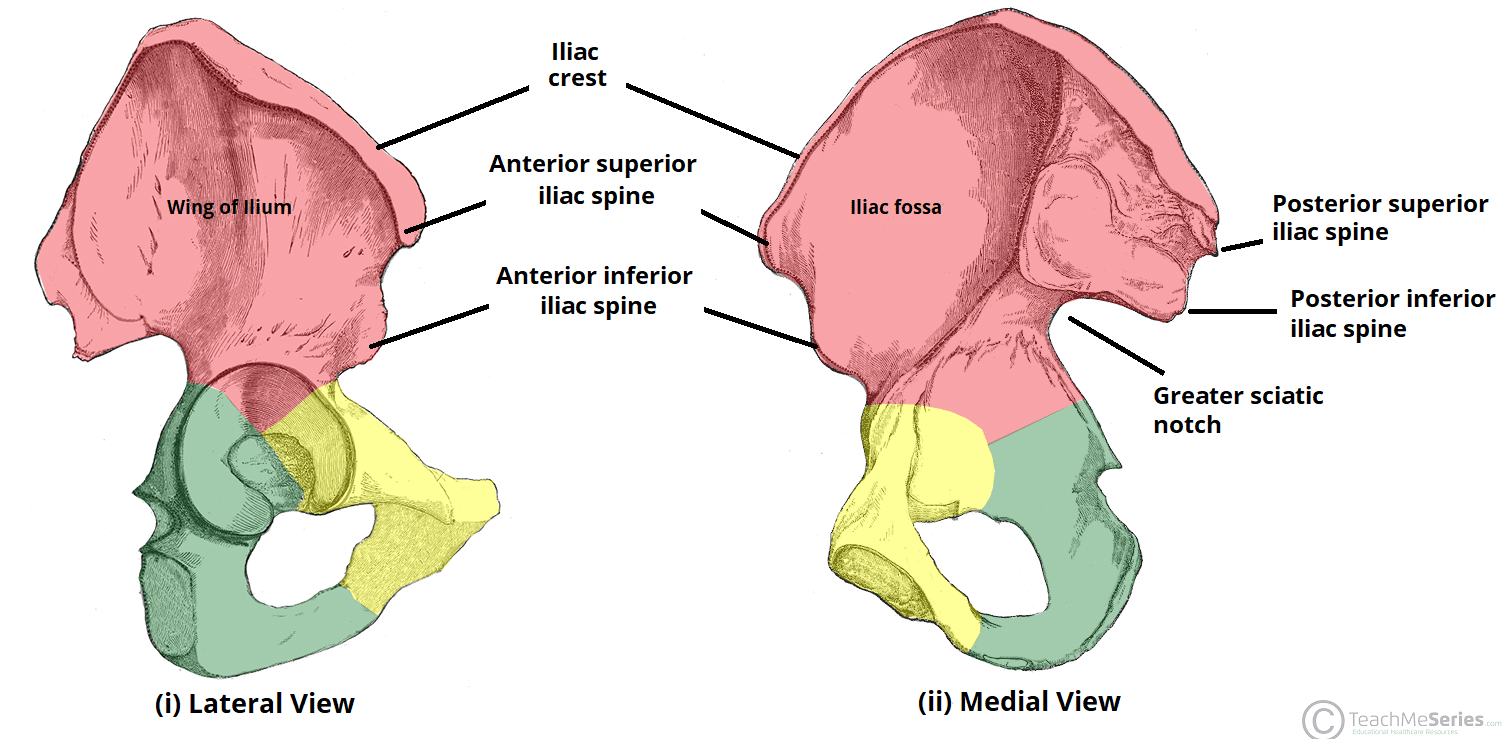
It also has two surfaces
- Internal: Smooth, curved surface (know as iliac fossa)
- External: Rough surface for gluteal muscle (muscle of the buttock) attachment
Anteriorly and posteriorly , the iliac crest ends in bony eminence called iliac spines, of importance is the posterior superior iliac spine which is found at the two small dim-ples on the right and left just above the cleft of the the buttocks while the posterior inferior iliac spine is where the sciatic nerves passes.
b. The Ischium (Bottom Back Part of Hip Bone)

This is the lowest part (infero-posterior ) of the innominate bone and forms the lower two-fifths of the acetabulum.
The ischial tuberosity is the body of the ischium, and it is upon the ischial tuberosities that we sit. About 2.5 cm (1 in.) above the ischial tuberosity is the ischial spine, which divides the greater and lesser sciatic notches, can be found.
During labor, midwives measure how far down the baby’s head has moved by comparing it to the ischial spines (checking baby’s progress through birth canal).
c. Pubic bone
The pubic bone forms the front part of the pelvis and the smallest bone of the innominate bone. It consists of two pubic bones joined anteriorly by the symphysis pubis, a cartilaginous joint that allows slight movement during childbirth. it joins with the ilium superiorly at and it joins with the Ischium inferiorly
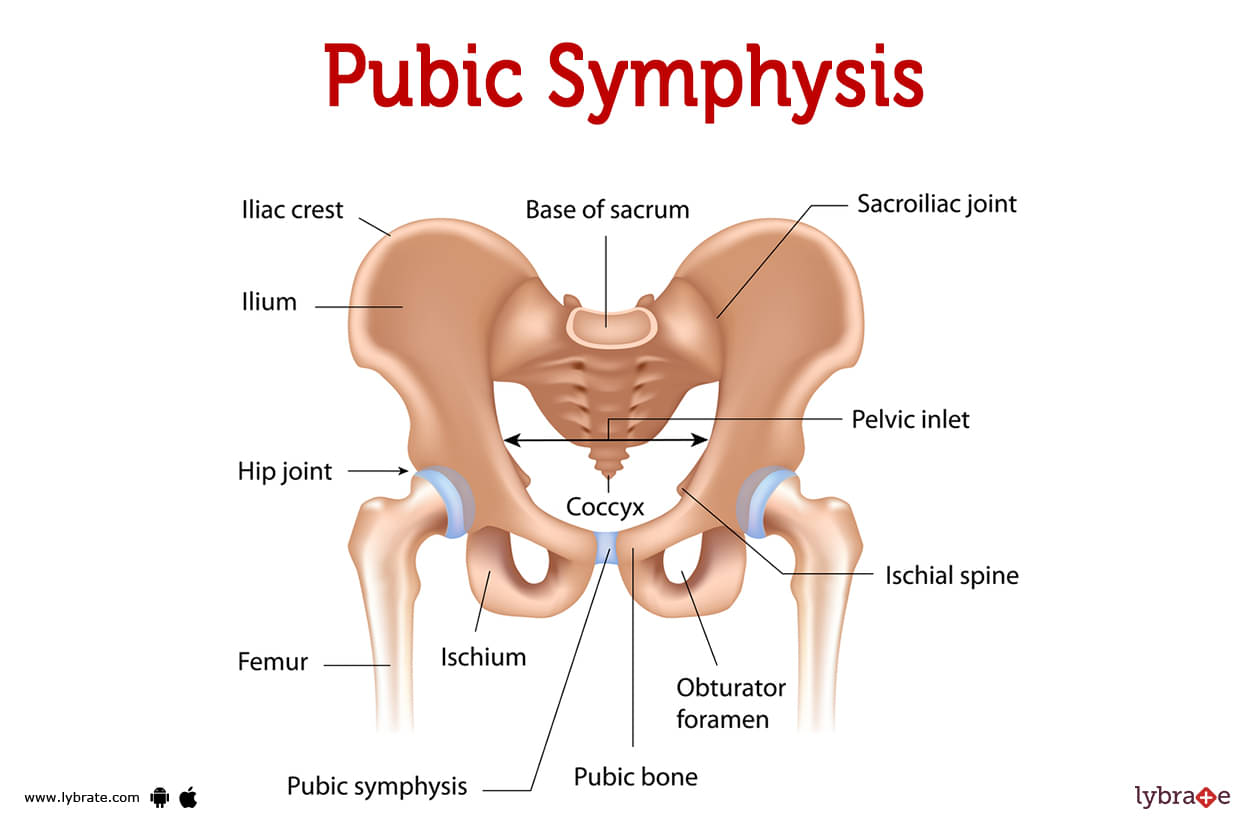
The pubic bone plays a crucial role in midwifery as it provide support and protection to the pelvic organs. Alos, The slight of the symphysis pubis helps accommodate the passage of the baby through the birth canal.
2. The Sacrum
The sacrum is a large, triangular bone made of five fused vertebrae. It forms the back wall of the pelvic cavity and connects to the iliac bones on each side to form the sacroiliac joints.
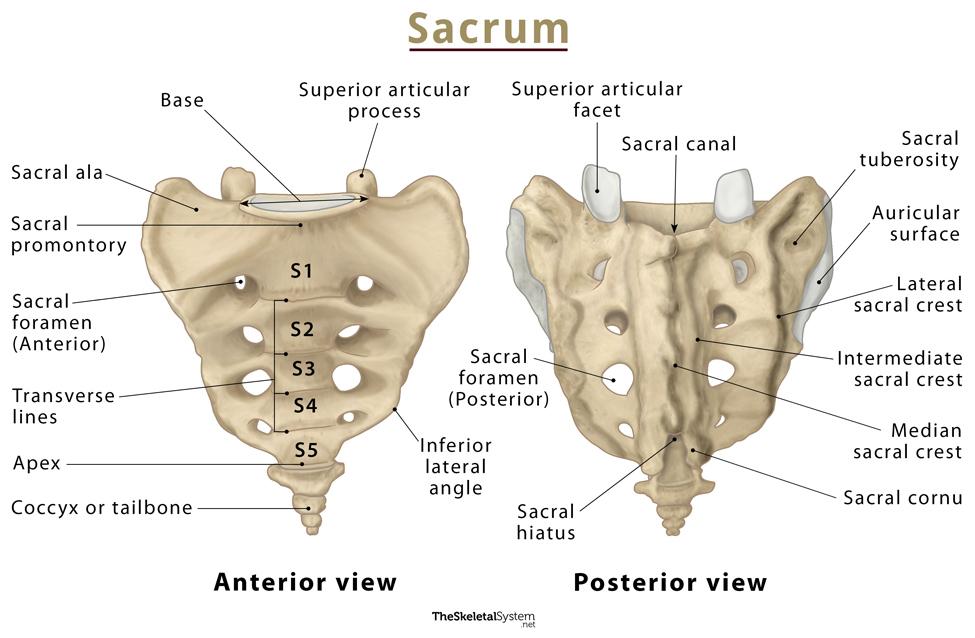
Key Features:
- At the top, the sacral promontory meets the first lumbar vertebra.
- At the bottom, the sacrum connects to the coccyx (tailbone).
- Four pairs of sacral foramina (holes) run along the sides—these allow nerves, blood vessels, and lymphatics to pass through.
- The sacral canal runs down the center of the bone and ends at the fifth sacral vertebra. It serves as a passageway for part of the spinal cord and nerves.
- The ala (wing-like projections) extend from the top sides.
- The back surface is rough and bumpy, providing anchorage for muscles and ligaments.
Why It Matters in Childbirth: Local anesthetic can be given through the caudal canal—a space near the sacral canal—to block pain during labor. This is known as a caudal or epidural block, and it helps relieve contraction pain while keeping the mother alert and able to push.
3. The Coccyx (Tailbone)
The coccyx is a small, triangular bone made up of four fused vertebrae. It’s considered vestigial, meaning it’s a leftover from evolutionary ancestors who had tails.
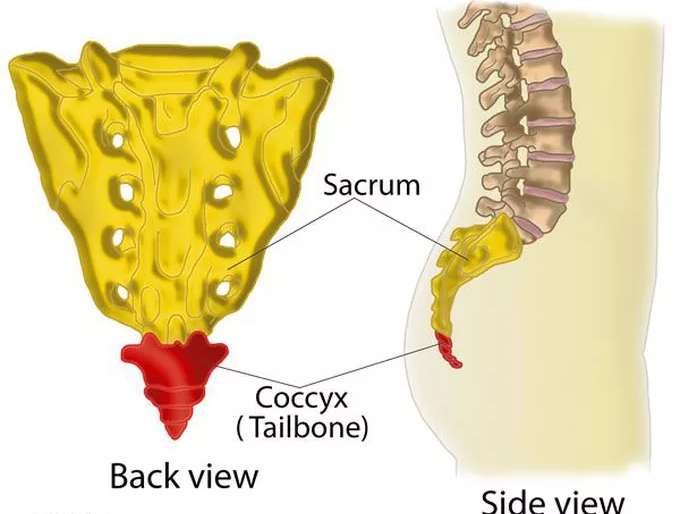
- Its base connects to the sacrum, and the tip points downward.
- Several pelvic muscles attach to it, including the external anal sphincter—the muscle that helps control bowel movements and other pelvic floor muscles that support posture and organ control
PELVIC JOINT
There are four main joints in the pelvis:
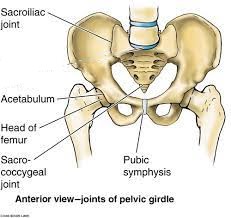
- Pubic Symphysis: A 4 cm cartilage pad located between the two pubic bones, reinforced by ligaments. It becomes more flexible in pregnancy to allow the bones to slightly separate during birth.
- Two Sacroiliac Joints: These connect the sacrum to the ilium (hip bones). They are strong, weight-bearing joints that allow minimal movement. During pregnancy, they enable a slight tilting or “nodding” of the sacrum, helping the pelvis adjust for labor.
- Sacrococcygeal Joint: Found between the sacrum and the coccyx (tailbone). It allows the coccyx to move backward during labor, creating more space in the pelvic outlet.
During pregnancy, the hormone relaxin softens these joints, allowing more mobility in the pelvic area. This slight movement is known as the “give of the pelvis”—a natural flexibility that helps the baby pass through the birth canal more easily.
Pelvic Ligaments
Pelvic ligaments support and stabilize the joints. Normally, they restrict movement, but under the influence of relaxin, they loosen gradually in pregnancy. This softening increases pelvic flexibility—also contributing to the give of the pelvis.
Main pelvic ligaments include:
- Sacroiliac Ligaments – Connect the sacrum to the ilium.
- Sacrotuberous Ligaments – Run from the sacrum to the ischial tuberosity.
- Sacrospinous Ligaments – Connect the sacrum to the ischial spine.
- Sacrococcygeal Ligaments – Link the sacrum and coccyx.
- Pubic Ligaments – Stabilize the pubic symphysis.
Some sources group the sacrotuberous and sacrospinous ligaments together, counting them as one unit—thus listing four major ligament groups.
The inguinal ligament (Poupart’s ligament), stretching from the anterior superior iliac spine to the pubic bone, forms the groin. It has no direct role in childbirth.
Divisions of the Pelvis
The pelvis is divided into two:
- False Pelvis: Located above the pelvic brim. Formed by the flared upper parts of the iliac bones, it supports and protects abdominal organs.
- True Pelvis: Below the brim. It contains the brim, cavity, and outlet—this is the space through which the fetus passes during delivery.
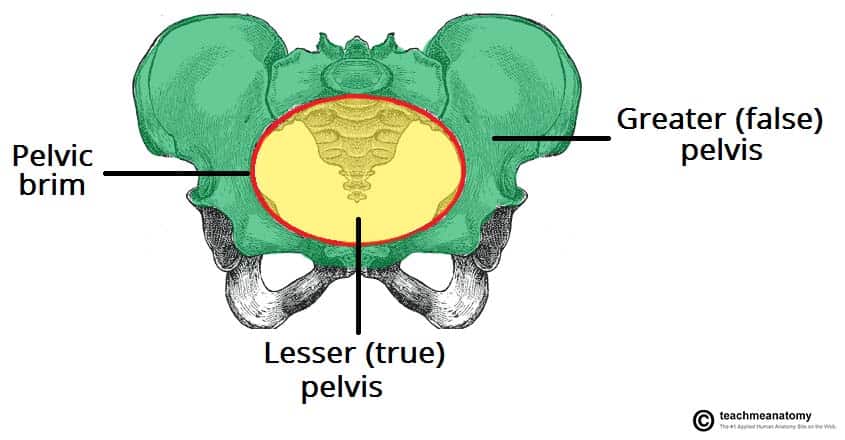
Pelvic Brim
The brim marks the entrance to the true pelvis and is usually round in females unless the sacral promontory protrudes.
Landmarks of the pelvic brim include:
- Promontory of the sacrum
- Ala of the sacrum
- Sacroiliac joint
- Iliopectineal line
- Iliopectineal eminence
- Superior ramus of the pubic bone
- Upper inner border of the pubic bone
- Upper inner border of the symphysis pubis
🧠 Pelvic Cavity
The pelvic cavity is the hollow, bowl-shaped space inside the true pelvis. It holds important organs and forms the passageway for the baby during childbirth.
🧍♀️ Organs Located in the Pelvic Cavity:
- Rectum – at the back, sitting in the curve of the sacrum and coccyx
- Bladder – at the front, just behind the pubic bone
- Pelvic colon – part of the large intestine
- Reproductive organs – such as the uterus and vagina in females
Pelvic Outlet (Birth Exit)
The pelvic outlet is the lower opening of the true pelvis. It’s where the baby finally exits the pelvis during birth.
There are two ways to define it:
1. Anatomical Outlet (Bone Structure Only)
This is made up of fixed bony landmarks:
- Lower border of the symphysis pubis
- Inferior pubic rami (inferior part of the pubic)
- Ischial tuberosities
- Sacrotuberous ligaments
This outlet is diamond-shaped and doesn’t change — it gives us a general idea of the space available. These landmarks are helpful for pelvimetry (measuring the pelvis) and assessing pelvic adequacy for childbirth.
2. Obstetrical Outlet (Practical Space for Birth)
This is clinically more important because it’s the actual space the fetus must pass through during delivery.
It includes a narrow zone called the pelvic strait, which is bordered by:
- The sacrococcygeal joint (where sacrum meets tailbone)
- The two ischial spines
- The lower edge of the symphysis pubis
The obstetrical outlet is the space between this narrow strait and the anatomical outlet — it’s what midwives and doctors are really assessing when checking for delivery readiness.
🧠 Note: Although the bones may seem rigid, the coccyx can tilt backward, and the pelvic ligaments stretch (thanks to relaxin), giving extra room for the baby’s head. This flexibility is called the “give of the pelvis.”
Pelvic Measurements
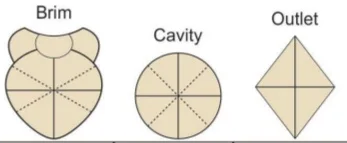
Several important pelvic dimensions help determine if the pelvis is adequate for childbirth. These measurements focus on three main levels: the pelvic brim, pelvic cavity, and pelvic outlet.

A – represent the anterior -posterior position
B – represent Diagonal position
C – represent Tranverse position
| Measurement | Brim | Cavity | Outlet |
|---|---|---|---|
| Antero-posterior (AP) | 11 cm (4 in.) | 12 cm (4.4 in.) | 13 cm (5 in.) |
| Oblique | 12 cm (4.3 in.) | 12 cm (4.4 in.) | 12 cm (4.4 in.) |
| Transverse | 13 cm (5 in.) | 12 cm (4.4 in.) | 11 cm (4 in.) |
Anterior-Posterior Measurement: This refers to the distance measured from the front (anterior) to the back (posterior) of the pelvic brim, cavity, or outlet.
Oblique Measurement: This is the diagonal distance between the pelvic brim points, usually from one sacroiliac joint to the opposite iliopubic eminence.
Transverse Measurement: This is the horizontal distance across the pelvis, measured side-to-side.
Planes of the pelvis
Planes of pelvis are imaginary flat surfaces drawn at the brim, cavity and outlet.
plane of the brim : marks the boundary between the false and true pelvis
Planes of the cavity- the planes with the greatest pelvic dimension. passes through t he third sacral vertebra and the midpoint of the symphysis pubis
Planes of the outlet – the planes with the least pelvic dimension passes through the lower border of the sacrum and the lower boarder of the symphysis
Axis of the Pelvis
It is also called the curve of Carus, It is an imaginary line intersecting each of these planes at right angles and is believed to represent the route the fetus follows while moving through the birth canal.
Inclination of the Pelvis
The pelvic brim’s plane forms a 60° angle with the floor when a person is standing upright. Since the pelvis is shaped like a curved canal, the angles of the brim, the cavity, and the outlet vary accordingly as follows:
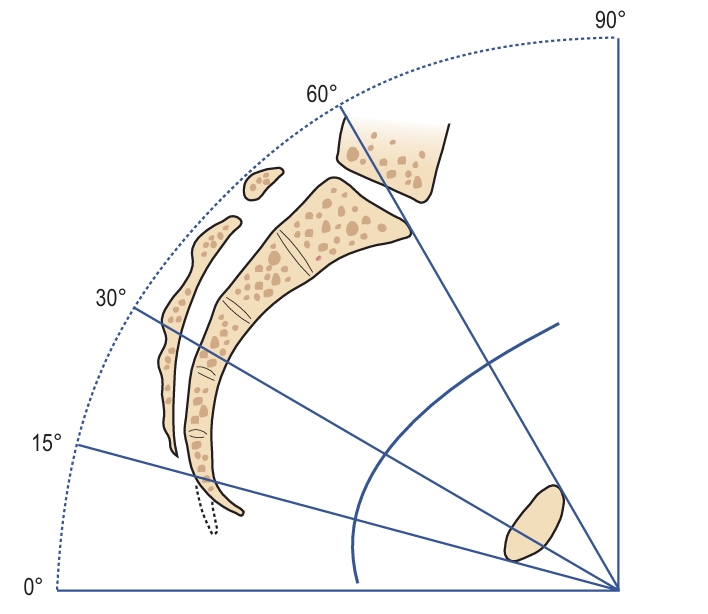
- The pelvic brim plane with the floor: 60°
- The pelvic cavity plane with the floor: 30°
- The pelvic outlet plane with the floor: 0°
Types of Pelvis
There are four main classifications of the female pelvis:
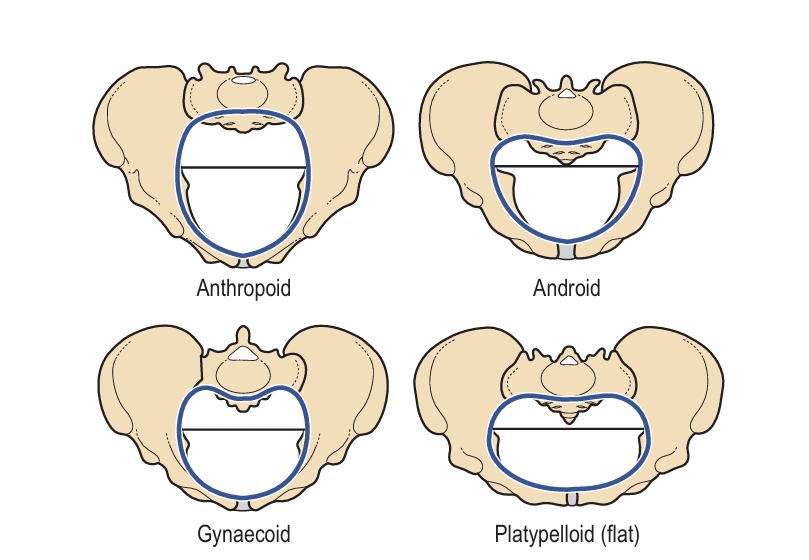
Gynecoid Pelvis
This is the typical female pelvis shape—round and wide, and well-suited for childbirth. It has a well-curved sacrum, along with a spacious pelvic brim and outlet, allowing for the easier passage of the baby during delivery.
Android Pelvis
Resembling the male pelvis, it is heart-shaped and narrower. The pelvic inlet is more triangular, which can lead to prolonged labor. Cesarean sections are more common with this pelvic type, especially if the baby is larger or in an unfavorable position. Manual rotation of the head and instrumental delivery may be attempted, depending on fetal size, position, and the degree of pelvic narrowing.
Anthropoid Pelvis
This pelvis has an oval-shaped brim with a larger anteroposterior diameter. It is narrower from side to side but longer front to back, which can often facilitate easier childbirth compared to the android pelvis. Labor usually does not present major difficulties, and vaginal delivery is often possible, though babies may need to rotate their heads differently as they pass through the birth canal.
Platypelloid Pelvis
This pelvis is flat and broad, with a wide transverse diameter but a short anteroposterior diameter. It has a kidney-shaped pelvic brim and can complicate labor due to its shape. With good uterine contractions, engagement may require lateral tilting of the head—a condition known as asynclitism—to allow the biparietal diameter to pass through the narrow anteroposterior brim. This can occasionally result in face presentation. If the pelvic brim is significantly contracted, Cesarean section is often required, although vaginal delivery may still be possible if the baby is small and well-positioned.