Neonatal jaundice is a common condition affecting newborns, marked by a yellow discoloration of the skin and sclera (eyes) due to high levels of bilirubin in the blood. Understanding this condition is essential for early identification and management to prevent complications. Recent data indicates that around 50-60% of full-term infants and up to 80% of preterm infants develop jaundice within the first week of life, with approximately 7-10% of exclusively breastfed infants continuing to show signs of jaundice at one month old.
What is Neonatal Jaundice?
Neonatal jaundice occurs when there is an accumulation of unconjugated bilirubin in the newborn’s bloodstream. Bilirubin is a yellow pigment formed during the breakdown of red blood cells. In newborns, the liver is often immature and less efficient at processing bilirubin, leading to its buildup.

Causes of Neonatal Jaundice
Neonatal jaundice can be physiological or pathological.
The role of midwife here is to detect and differentiate between physiology and pathological jaundice by the timing and clinical presentation to instigate appropriate management.
1. Physiological jaundice
This common condition usually appears between the second and fifth day of life, peaking around days three to five. It resolves as the baby’s liver matures and becomes better at processing bilirubin, which is produced from the normal breakdown of fetal hemoglobin. The condition does not show up before 24 hours after birth and typically resolves within 10-12 days. Although generally harmless, it is important to monitor bilirubin levels to avoid complications if they rise too high.
Pathophysiology / causes of physiological jaundice
Babies usually look normal on their first day but can develop jaundice by days 3-4 due to rising levels of unconjugated bilirubin. As bilirubin builds up, it saturates serum albumin and spills into the blood plasma, depositing in the subcutaneous fat (being fat soluble) , which cause the skin to turn yellow. This fat-soluble bilirubin when saturated can also cross the blood-brain barrier and deposit in the brain, which may lead to brain damage and long-term issues like cerebral palsy and learning difficulties. Fortunately, cases of bilirubin encephalopathy are now rare because of improvements in treatment, such as phototherapy and exchange transfusion, as well as a decrease in Rhesus hemolytic disease.
2. Pathological jaundice
On the other hand, jaundice may appear within the first 24 hours of life or persist beyond two weeks. It is characterized by a rapid increase in serum bilirubin levels. This Prolonged or early-onset jaundice may indicate underlying conditions that require further evaluation and management.
Causes of Pathological Jaundice
this will be classified based on early and late neonatal jaundice
a. Early Neonatal Jaundice (<24 hours)
- Hemolytic causes
- Blood group incompatibilities (ABO, Rh)
- Hemoglobinopathies (e.g., hereditary spherocytosis)
- Inherited enzyme deficiencies (e.g., G6PD deficiency)
- Birth trauma
- Bruising or cephalohematoma leading to increased bilirubin load
- Polycythemia
- Increased red cell mass causing higher breakdown
- Infections
- Severe neonatal sepsis (may present early)
Note: Among all these causes, hemolytic causes are the most common. This condition is also referred to as hemolytic jaundice.
what is Heamolytic jaundice
jaundice within the first 24 hours after birth is assumed to be due to haemolysis until proven otherwise. Haemolysis is increased haemoglobin destruction in the fetus or newborn and has several causes, the most important being blood group incompatibility. This
can occur due to various antibodies, but the most important is caused by Rhesus (Rh-D) isoimmunization/incompatibility.
When a baby develops jaundice in the first 24 hours after birth, hemolysis (breakdown of red blood cells) is considered to be the cause until it is ruled out by other causes are ruled out. Hemolytic jaundice happens when red blood cells are destroyed too quickly in the fetus (baby’s body). The main cause is when the mother’s and baby’s blood types don’t match properly. This creates a problem where the mother’s antibodies attack the baby’s red blood cells. The most serious type occurs with Rhesus (Rh) blood group differences, where an Rh-negative mother carries an Rh-positive baby, leading to severe jaundice that needs immediate treatment. this is known as Rhesus (Rh-D) isoimmunization/incompatibility. Other cause could be ABO incompatibility
- Rhesus (Rh-D) isoimmunization/incompatibility.
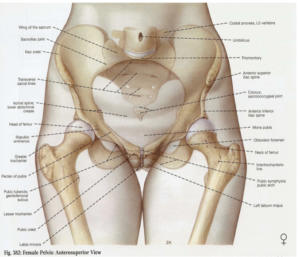
Rhesus (Rh) incompatibility develops when an Rh-negative mother is exposed to Rh-positive fetal red blood cells that cross into her circulation. Her immune system treats the D antigen as a foreign substance, triggering antibody production. These maternal antibodies can then pass through the placenta and attack the baby’s red blood cells, causing their destruction.
This represents a critical condition where midwives play an essential role by ensuring anti-D immunoglobulin (anti-D Ig) is given within 72 hours following delivery. Failure to provide this preventive treatment can result in Rh-D sensitization, potentially causing hemolytic disease of the newborn (HDN) in future pregnancies, which carries substantial risks of serious complications and death for affected infants.
- ABO isoimmunization
ABO isoimmunization, also known as ABO incompatibility, occurs when a pregnant woman has a different ABO blood type than her fetus. This condition arises when the mother has type O blood and the fetus has either type A or type B blood.
In such cases, the mother may produce antibodies against the A or B antigens present on the fetal red blood cells. If these antibodies cross the placenta, they can attack the fetal red blood cells, leading to hemolytic disease of the newborn (HDN). This can result in various complications, including jaundice, anemia, and in severe cases, hydrops fetalis or stillbirth.
Management of ABO isoimmunization typically involves monitoring the fetus for signs of anemia and jaundice during and after pregnancy. If necessary, treatments may include intrauterine blood transfusions or phototherapy after birth to manage jaundice. In most cases, ABO incompatibility is less severe than Rh incompatibility, but it still requires careful monitoring and management.
b. Late neonatal jaundice (> 14 days)
This is typically defined as a persistent elevation of bilirubin levels beyond 14 days of life. It refers to the yellow discoloration of the skin and eyes in a newborn that appears after the first week, commonly between one to two weeks of age. While jaundice is often normal in newborns due to their immature liver function, a late onset may signal underlying medical issues that require evaluation.
The causes of late neonatal jaundice can be broadly categorized into two groups based on the type of bilirubin involved:
1. Late Neonatal Unconjugated (Indirect, Fat-Soluble) Hyperbilirubinemia (>14 days)
This form usually involves:
- Inadequate breastfeeding or insufficient milk intake
- Hemolytic conditions such as ABO or Rh incompatibility
- Inherited enzyme deficiencies, for example, glucose-6-phosphate dehydrogenase (G6PD) deficiency
- Hypothyroidism
- Infections such as sepsis
- Metabolic disorders like galactosemia
2. Late Neonatal Conjugated (Direct, Water-Soluble) Hyperbilirubinemia (>14 days)
Conjugated hyperbilirubinemia should be suspected particularly if there are pale stools and dark urine. Important causes include:
- Biliary atresia
- Conditions causing dehydration, starvation, hypoxia, or sepsis, as oxygen and glucose are essential for bilirubin conjugation
- TORCH infections (toxoplasmosis, rubella, cytomegalovirus, herpes, and others)
- Other viral infections such as neonatal viral hepatitis
- Bacterial infections, especially those caused by E. coli
- Metabolic and endocrine disorders affecting the enzyme UDP-glucuronosyltransferase (UDPGT), including Crigler–Najjar syndrome and Gilbert’s syndrome
- Other metabolic disorders, including hypothyroidism
General symptoms of Neonatal jaundice
The hallmark sign of neonatal jaundice is the yellowing of the skin and eyes, which typically starts on the face and progresses downward. Other symptoms may include poor feeding, lethargy, or high-pitched crying, which require immediate medical attention.

Management of Neonatal jaundice
Physical Assessment
- Observe for changes in skin and scleral colour
- Check for skin bruising or cephalhaematoma
- Assess for other clinical signs such as lethargy and decreased eagerness to feed
- Check for dehydration
- Consider signs of infection including temperature changes, vomiting, irritability, or high-pitched cry
- Observe for dark urine and light stools, which could indicate intrahepatic or extrahepatic obstructive disease
Laboratory investigations
- Always measure serum bilirubin (SBR).
If bilirubin levels are elevated as in the case of pathological jaundice, perform additional tests including:
- Direct Coombs test (DCT) to identify maternal antibodies attached to the infant’s red blood cells
- Blood typing and Rh factor analysis for both the infant and mother to check for incompatibility
- Hemoglobin measurement to evaluate for anemia or polycythemia
- WBC count to detect infection
- urine for substance such as galactose
- Conjugated bilirubin assessment if signs indicate possible conjugated hyperbilirubinemia
Treatment strategy
- Phototherapy: The primary treatment exposes the baby to blue light, which converts bilirubin into a water-soluble form that the body can eliminate through urine. It is most effective for physiological jaundice. If phototherapy lights are unavailable, sunlight might be used cautiously as a last resort.
- Immunogobulin: Infusing a set volume of pooled human immunoglobulin helps prevent the need for exchange transfusion in pathological jaundice like hemolytic disease. It works by neutralizing excess antibodies, reducing the rapid rise of bilirubin caused by red blood cell destruction.
- Exchange Transfusion: In severe cases where phototherapy and hydration fail, exchange transfusion rapidly lowers bilirubin by simultaneously removing baby’s blood and transfusing a large volume of blood to the baby, often through an umbilical venous catheter. This procedure is performed when bilirubin levels exceed safe threshold.
- Supportive care: Ensuring adequate breast feeding helps promote bilirubin excretion through stools.
Prevention and Education
Antenatal screening for blood group incompatibilities and educating parents on recognizing early signs of jaundice is essential. Early feeding, frequent monitoring, and timely intervention are key to preventing complications.
Neonatal jaundice, while common, requires careful monitoring and appropriate management to ensure the health and safety of the newborn. Healthcare providers and parents can work together to identify jaundice early, understand its causes, and apply effective treatments to safeguard newborn wellbeing.